So that everything runs smoothly: Focusing on cartilage tissue
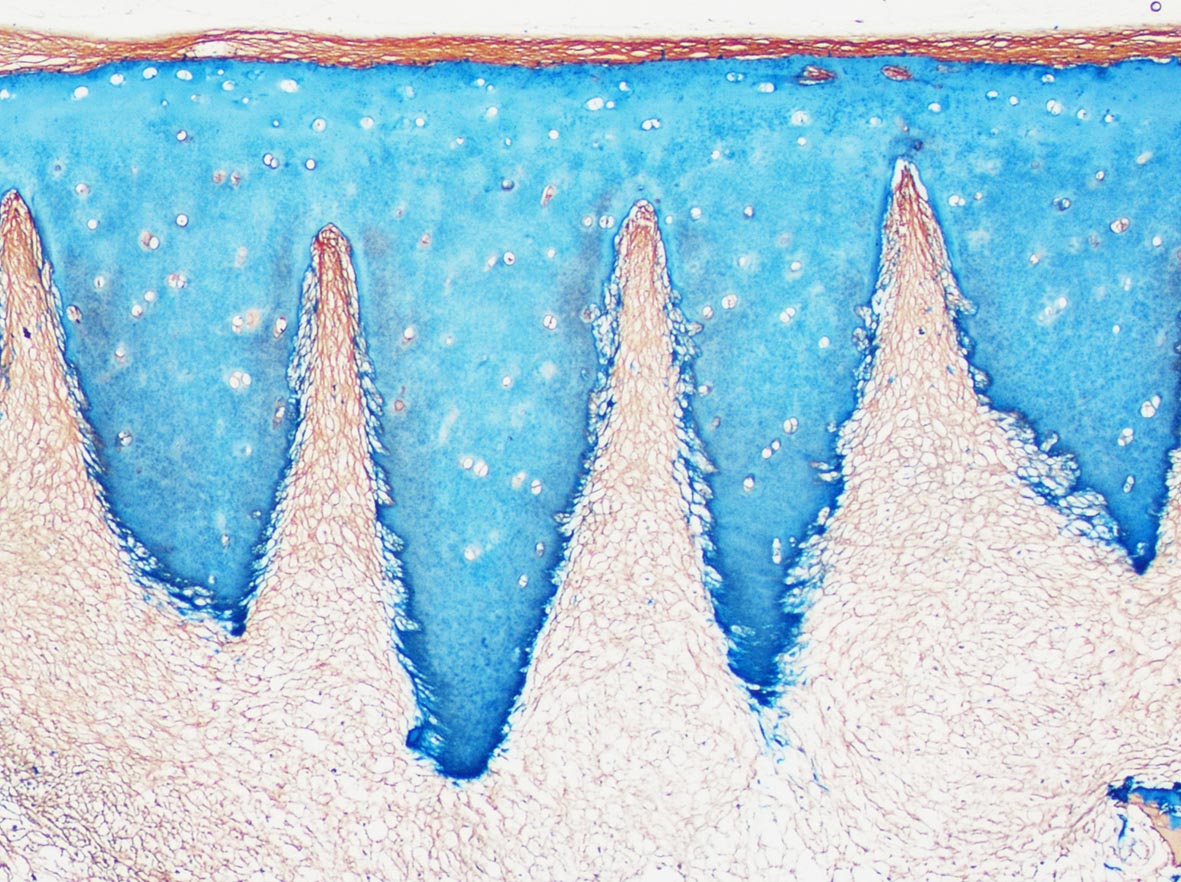
At first glance, articular cartilage is a particularly simple tissue. It consists of just one type of cell, called chondrocytes, embedded in a collagen matrix, free of nerves or blood vessels. As a thin layer at the end of bones, it ensures that we can move smoothly and that shocks are cushioned.
But it is precisely this simplicity that can become a disaster in joint injuries. When cartilage tissue is lost, a lesion is left behind that cannot regenerate on its own because there are hardly any cells to build new tissue. Over time, the condition worsens progressively and, if left untreated, leads to painful joint arthrosis.
To regenerate cartilage defects caused by injury, the patient’s own cells are introduced into the defect in the course of a surgical intervention, either stem cells from the underlying bone marrow or chondrocytes taken through a small biopsy and multiplied in the laboratory. Biomaterials are often used to support the cells, their distribution and protection. In most cases, this treatment leads to a significant improvement in the clinical symptoms of the patients, but not to a complete restoration of the original situation. Research has shown that materials currently used in the clinic do not adequately reflect the composition and architecture of hyaline cartilage.
The cartilage regeneration research group at the Ludwig Boltzmann Institute for Experimental and Clinical Traumatology, AUVA Research Centre, led by Sylvia Nürnberger (Department of Orthopaedics and Trauma Surgery at the Medical University Vienna) was able to show that the natural cartilage matrix is more suitable as a biomaterial for cartilage regeneration. This is because the tissue, which at first glance appears to be very simple, is in fact highly specialised in its natural form. The collagen fibres are perfectly adapted to their function as shock absorbers in a complex network.
The patient’s own cartilage is only available as a filling material to a very limited extent. However, cartilage is routinely removed during operations and can be used as donor cartilage. The donor cells, which could cause an immune reaction, are then degraded and removed in several steps.
“This leaves a very dense matrix, but patient cells cannot migrate into it. The opening of the matrix was the technological challenge of this development and was achieved with laser processing. This allowed us to make the finest notches in a controlled and standardised way to make even deeper tissue regions accessible for regenerative cells,” explains Nürnberger. “The developed material largely resembles the initial cartilage in structure and composition and can therefore serve as a component of the regenerative tissue and thus supports the tissue formation process.”
These properties distinguish the newly developed material “CartiScaff” from previous approaches and give hope for faster and more sustainable regeneration. In colonisation trials with cartilage cells, bone marrow cells and stem cells from adipose tissue, it was shown that CartiScaff promotes the formation of particularly high-quality regenerative tissue. The innovative invention was made possible by support from the Austrian Research Promotion Agency FFG and the Lorenz Böhler Fund. The first study recently appeared in EBiomedicine, an open access journal published by The Lancet.
In a follow-up study, the material is currently being tested for its suitability under a near-clinical stress situation. It is hoped that the new biomaterial can be used in the future with common surgical methods and will extend and improve conventional therapies.
Laser-treated cartilage from tissue donors is only one of the options the group is researching. This is because the immigration of cells into the extraordinarily densely packed cartilage matrix has been a challenge for scientists for years.
In a study published in 2018 in the renowned Acta Biomaterialia, the scientists succeeded for the first time worldwide in uniformly repopulating cartilage with an intact collagen structure. Instead of articular cartilage, they used ear cartilage donated by the Silmbroth butcher’s shop in Scharnstein im Almtal (Upper Austria). In addition to collagen and proteoglycans, this cartilage also contains elastic fibres that are not found in articular cartilage. If these fibres are removed enzymatically, a network of channels is exposed that runs through the entire matrix and allows the cells access to deep tissue layers. In these channels, cells form regenerative tissue with typical cartilage characteristics within a few weeks.